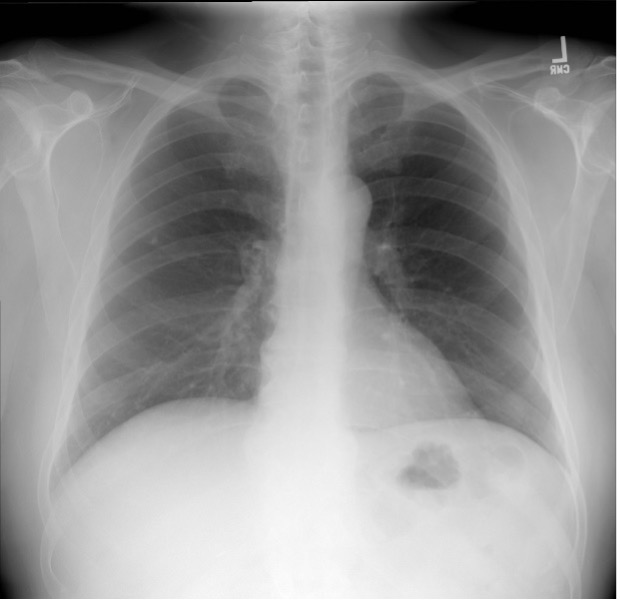
A 61-year-old woman with mild persistent asthma controlled with inhaled corticosteroids and an as needed albuterol inhaler presents to the emergency department with shortness of breath and audible “wheezing” for approximately 5-7 days after a total thyroidectomy for papillary carcinoma of the thyroid. The difficulty with breathing has steadily worsened, despite increasing use of albuterol. She reports a tingling sensation around the mouth and numbness in her hands and feet with sporadic muscle cramps mainly in the legs throughout the day and especially at night. On physical examination, she appears to be in mild respiratory distress, with a respiratory rate of 22 breaths/min, using some accessory muscles, and not being able to finish all her sentences. Lung examination is significant for expiratory wheezing throughout all fields. A chest radiograph is performed (see figure below). An arterial blood gas is drawn and shows a pH of 7.36, PCO2 of 40 mm Hg, and PO2 of 90 mm Hg on 2 L nasal cannula oxygen. The patient is given intravenous glucocorticoids and continuously nebulized albuterol and ipratropium. Despite this, she remains symptomatic with audible stridor.
Which of the following is the most appropriate next step in the treatment for this patient’s respiratory symptoms?
A) Calcium chloride or calcium gluconate intravenously
Although this patient has mild persistent asthma, she also recently had a total thyroidectomy, placing her at risk for hypocalcemia from hypoparathyroidism. Even without inadvertent parathyroid gland removal, transient hypoparathyroidism occurs in 10% of patients who undergo total thyroidectomy. Hypoparathyroidism results in hypocalcemia because without parathyroid hormone, the body cannot mobilize calcium from bone or reabsorb calcium from the gastrointestinal tract or kidney. Hypocalcemia usually occurs in the first few days after surgery and can cause paresthesias, muscle cramps and spasms, or tetany. More serious effects include seizures, cardiac arrhythmias, laryngospasm, and bronchospasm which may reflect tetany of the bronchial smooth muscle. Severe hypocalcemia should be corrected rapidly, so a bolus of intravenous calcium should be administered.
Answer choice B: Double the dose of the intravenous glucocorticoids, is incorrect. While corticosteroids help reduce inflammation and are beneficial in patients with asthma exacerbations, the failure to respond to continuous bronchodilators and intravenous steroids makes this less likely an asthma exacerbation. Therefore, higher dosing is not needed at this time.
Answer choice C: Emergent intubation, is incorrect. Some patients who present with severe, refractory asthma exacerbations may need mechanical ventilation. This patient needs to be closely monitored, but if her symptoms are secondary to hypocalcemia she would quickly respond to the intravenous calcium, avoiding the need for invasive mechanical ventilation.
Answer choice D: Start intravenous aminophylline and answer choice E: Start intravenous terbutaline, are incorrect. These are not recommended treatments for asthma exacerbation including status asthmaticus and should not be used. Also, this patient is not having a refractory asthma attack but rather the clinical manifestations of presumed hypocalcemia.
Key Learning Point
Transient hypoparathyroidism occurs in 10% of patients who undergo total thyroidectomy. Presenting symptoms include paresthesias, muscle cramps and spasms, or tetany. More serious effects include seizures, cardiac arrhythmias, laryngospasm, and bronchospasm. Severe hypocalcemia should be corrected rapidly with intravenous calcium.